RFK Jr.: ‘We will act’ on petition to regulate ultra-processed foods
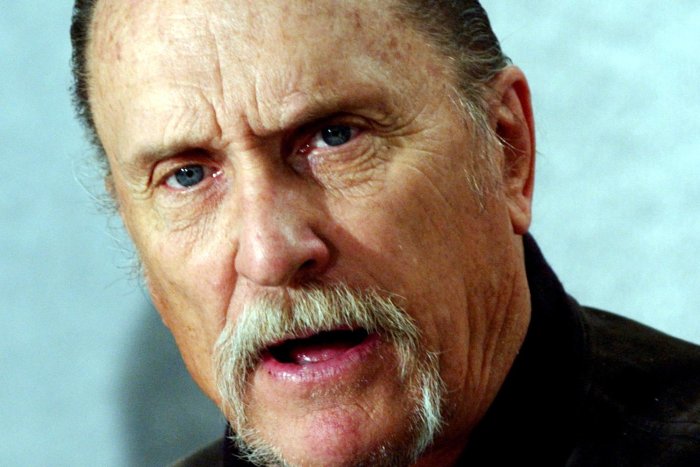
Feb. 16 (UPI) — Health and Human Services Secretary Robert F. Kennedy Jr. plans to take action on a petition calling for increased regulations on ultra-processed foods.
Kennedy said in an interview on CBS News’s 60 minutes on Sunday that he wants to address concerns raised by a citizen petition to the Food and Drug Administration. The petition seeks to limit exposure to ultra-processed foods and ingredients to prevent the risks of obesity, diabetes and cardiovascular disease.
“There is no way for any American to know if a product is safe if it is ultra processed,” Kennedy said.
The petition seeks to make changes to the “Generally recognized as safe” exemption that allows food companies to verify the safety of foods and ingredients independently. Changes would include revoking the allowance of processed refined carbohydrates in food processing and removing such products from the shelves unless specifically authorized.
Kennedy said the exemption is a loophole that has allowed food companies to introduce “thousands upon thousands of new ingredients into our food supply.”
“This agency does not know how many ingredients there are in American food,” Kennedy said.
Kennedy clarified that it has not been determined that the Trump administration will regulate ultra-processed foods. The term “ultra-processed food” has not been defined by federal regulators.
Former FDA Commissioner David Kessler authored the petition. Kessler served under presidents George H.W. Bush and Bill Clinton and was involved with “Operation Warp Speed” during the COVID-19 pandemic.
Kessler defined ultra-processed foods as refined sweeteners, refined flours and starches, and added fats and oils and salt. However, his petition is focused on refined sweeteners, flours and starches, which are processed refined carbohydrates.
Refined sweeteners include ingredients like high fructose corn syrup, glucose syrup and dextrose.
“These processed refined carbohydrates are central to the widespread availability of ultraprocessed foods,” Kessler writes. “This petition focuses on processed refined carbohydrates that are primary causal determinants of metabolic harm.”