The harsh truth about HIV phobia in gay dating
“Internalized stigma is what occurs when applying the stereotypes about who gets HIV, the prejudice, the negative feelings, onto yourself,” says Smith.
In 2024, 38% of people living with HIV reported internalized stigma. And studies show that it can predict hopelessness and lower quality of life, even when people are engaged in care or virally suppressed.
Internalized stigma can also affect how people practice safe sex and communicate about the virus. A 2019 survey of men who have sex with men found that individuals who perceived greater community-level stigma were less likely to be aware of—and use—safer-sex functions available on dating apps, such as HIV-status disclosure fields, as well as sexual health information and resources.
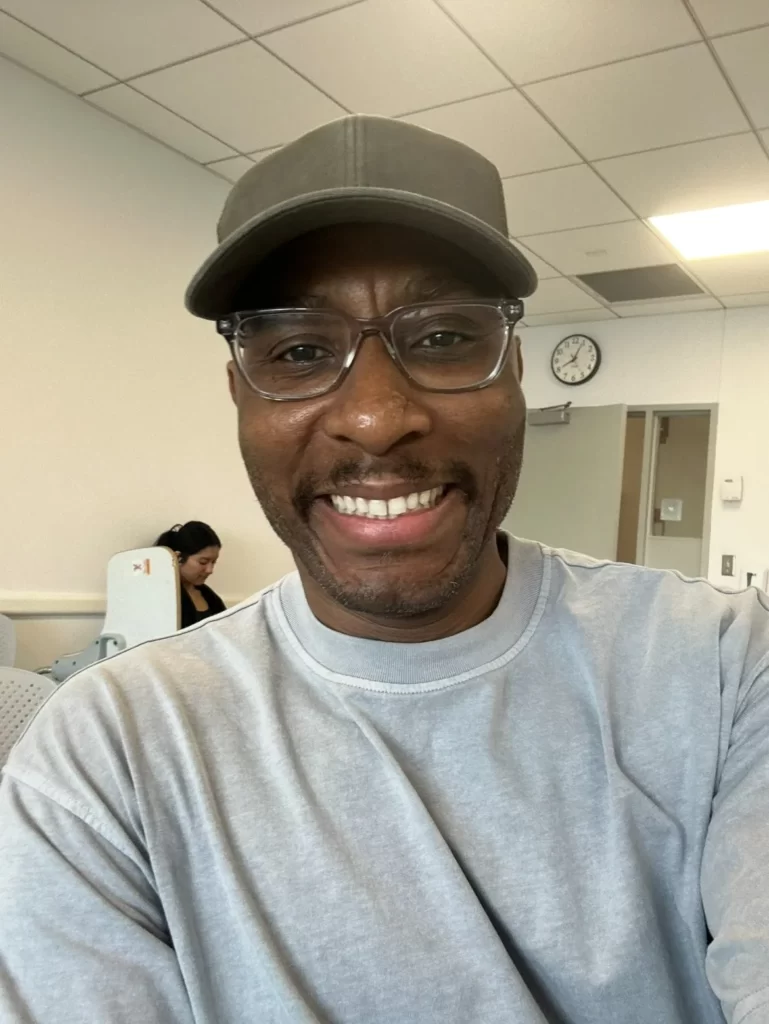
“[HIV phobia] is probably the most intense, subvert bigotry I think you could experience,” Joseph Monroe Jr., a 48-year-old living in the Bronx, told Uncloseted Media.

On dating apps, men have messaged him things like, “You look like you’ve got that thing” and “Go ahead and infect someone else.”
Monroe Jr. has also dealt with misinformed people who rudely opine about how he contracted the virus: “Who fucked you? That’s how you got it, right?” people will say to him.
“You end up internalizing all these stereotypes about who gets HIV—that you were promiscuous, that you didn’t care about yourself, that you did something wrong,” says Smith. “You carry that in, and then you have to relearn: ‘No, I didn’t. This is just a health condition.’”
What HIV Acceptance Looks Like and Raising Awareness
For those living with HIV, acceptance feels far away.
“You’re living under this threat of HIV and the threat that others find you threatening. It inhabits you socially and sexually,” Koester says. “People are hunkering down. Not putting themselves out there and having a mediocre quality of life. To have a sense of empowerment, you have to be legitimate and seen in the world and it’s hard to do that with the stigma that exists.”

Researchers say the path forward lies as much in conversation as in medicine.
Koester says she talks about HIV and PrEP anywhere she can, including in salons, cafes and restaurants. “Whenever I get into a cab with someone, I’m going to bring up HIV so the driver gets accustomed to hearing about it. … We have a long way to go in terms of exposure and awareness and every little bit helps.”
Part of this lies in increasing awareness through targeted marketing campaigns. PrEP is still profoundly misunderstood outside major urban centers, with uneven uptake among minority groups and usage gaps in the bible belt. And a 2022 U.S. survey found that 54.5% of people living with HIV didn’t know what U=U meant, and less than half of Americans agree that people living with HIV who are on proper medications cannot transmit the virus.
While eradicating stigma is slow, there is hope for acceptance.

Years after Jack’s diagnosis, in 2021, he told a man he was on a third date with that he was HIV-positive but undetectable. His date’s reply was almost casual: “Oh—is that it? I thought you were going to say you had a boyfriend or something. I’m on PrEP. You’re fine.”
“It felt so good to hear him say that and accept me,” says Jack. “I was like, ‘This is my person. You’re my person.’” One year later, they got married.
Back in Florida, 19-year-old Cody Nester isn’t feeling this acceptance. He still scrolls past profiles that read “Only negative guys” and tries to ignore the hateful messages.
“It still hurts, but I know it’s coming from fear,” he says. “I wasn’t too informed about HIV before I got it. … When I got it, I really jumped into the rabbit hole and began to learn. I really do think [HIV and stigma] is because people are not knowledgeable. … When people don’t know details, they tend to get scared.”
Additional Reporting by Nandika Chatterjee.

If objective, nonpartisan, rigorous, LGBTQ-focused journalism is important to you, please consider making a tax-deductible donation through our fiscal sponsor, Resource Impact, by clicking this button: