California counties unsure how how they’ll pay for uninsured
In 2013, before the Affordable Care Act helped millions get health insurance, California’s Placer County provided limited healthcare to some 3,400 uninsured residents who couldn’t afford to see a doctor.
For several years, that number has been zero in the predominantly white, largely rural county stretching from Sacramento’s eastern suburbs to the shores of Lake Tahoe.
The trend could be short-lived.
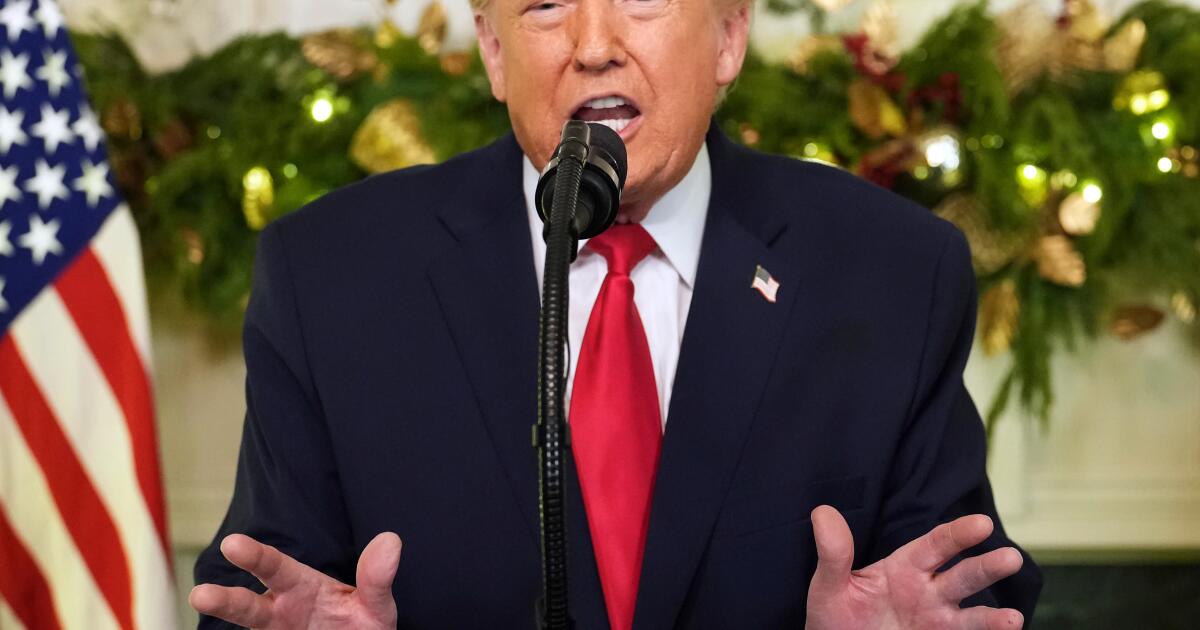
County health officials there and across the country are bracing for an estimated 10 million newly uninsured patients over the next decade in the wake of Republicans’ One Big Beautiful Bill Act. The act, which President Trump signed into law this summer, is expected to reduce Medicaid spending by more than $900 billion over that period.
“This is the moment where a lot of hard decisions have to be made about who gets care and who doesn’t,” said Nadereh Pourat, director of the Health Economics and Evaluation Research Program at UCLA. “The number of people who are going to lose coverage is large, and a lot of the systems that were in place to provide care to those individuals have either gone away or diminished.”
It’s an especially thorny challenge for states such as California and New Mexico where counties are legally required to help their poorest residents through what are known as indigent care programs. Under Obamacare, both states were able to expand Medicaid to include more low-income residents, alleviating counties of patient loads and redirecting much of their funding for the patchwork of local programs that provided bare-bones services.
Placer County, which estimates that 16,000 residents could lose healthcare coverage by 2028, quit operating its own clinics nearly a decade ago.
“Most of the infrastructure that we had to meet those needs is gone,” said Rob Oldham, Placer County’s director of health and human services. “This is a much bigger problem than it was a decade ago and much more costly.”
In December, county officials asked to join a statewide association that provides care to mostly small, rural counties, citing an expected rise in the number of uninsured residents.
New Mexico’s second-most populous county, Doña Ana, added dental care for seniors and behavioral health benefits after many of its poorest residents qualified for Medicaid. Now, federal cuts could force the county to reconsider, said Jamie Michael, Doña Ana’s health and human services director.
“At some point we’re going to have to look at either allocating more money or reducing the benefits,” Michael said.
Straining state budgets
Some states, such as Idaho and Colorado, abandoned laws that required counties to be providers of last resort for their residents. In other states, uninsured patients often delay care or receive it at hospital emergency rooms or community clinics. Those clinics are often supported by a mix of federal, state and local funds, according to the National Assn. of Community Health Centers.
Even in states like Texas, which opted not to expand its Medicaid program and continued to rely on counties to care for many of its uninsured, rising healthcare costs are straining local budgets.
“As we have more growth, more people coming in, it’s harder and harder to fund things that are required by the state Legislature, and this isn’t one we can decrease,” said Windy Johnson, program manager with the Texas Indigent Health Care Assn. “It is a fiscal issue.”
California lawmakers face a nearly $18-billion budget deficit in the 2026-27 fiscal year, according to the latest estimates by the state’s nonpartisan Legislative Analyst’s Office. Gov. Gavin Newsom, who recently acknowledged he’s mulling over a White House run, has rebuffed several efforts to significantly raise taxes on the ultrawealthy. Despite blasting the bill passed by Republicans in Congress as a “complete moral failure” that guts healthcare programs, the Democrat this year rolled back state Medi-Cal benefits for seniors and for immigrants without legal status after rising costs forced the program to borrow $4.4 billion from the state’s general fund.
H.D. Palmer, a spokesperson for the state’s Department of Finance, said that the Newsom administration is still refining its fiscal projections and that it would be premature to discuss potential budget solutions.
Newsom will unveil his initial budget proposal in January. State officials have said California could lose $30 billion a year in federal funding for Medi-Cal under the new law, as much as 15% of the state program’s entire budget.
“Local governments don’t really have much capacity to raise revenue,” said Scott Graves, a director at the independent California Budget & Policy Center with a focus on state budgets. “State leaders, if they choose to prioritize it, need to decide where they’re going to find the funding that would be needed to help those who are going to lose healthcare as a result of these federal funding and policy cuts.”
Reviving county-based programs in the near term would require “considerable fiscal restructuring” through the state budget, the Legislative Analyst’s Office said in an October report.
No easy fixes
It’s unclear how many people are enrolled in California’s county indigent programs, because the state doesn’t track enrollment and utilization. But enrollment in county health safety net programs dropped dramatically in the first full year of Affordable Care Act implementation, going from about 858,000 people statewide in 2013 to roughly 176,000 by the end of 2014, according to a survey at the time by Health Access California.
“We’re going to need state investment,” said Michelle Gibbons, executive director of the County Health Executives Assn. of California. “After the Affordable Care Act and as folks got coverage, we didn’t imagine a moment like this where potentially that progress would be unwound and folks would be falling back into indigent care.”
In November, voters in affluent Santa Clara County approved a sales tax increase, in part to backfill the loss of federal funds. But even in the home of Silicon Valley, where the median household income is about 1.7 times the statewide average, that is expected to cover only a third of the $1 billion a year the county stands to lose.
Health advocates fear that, absent major state investments, Californians could see a return to the previous patchwork of county-run programs, with local governments choosing whom and what they cover and for how long.
In many cases, indigent programs didn’t include specialty care, behavioral health or regular access to primary care. Counties can also exclude people based on immigration status or income. Before the ACA, many uninsured people who needed care didn’t get it, which could lead to them winding up in emergency rooms with untreated health conditions or even dying, said Kiran Savage-Sangwan, executive director of the California Pan-Ethnic Health Network.
Rachel Linn Gish, interim deputy director of Health Access California, a consumer advocacy group, said that “it created a very unequal, maldistributed program throughout the state.”
“Many of us,” she said. “including counties, are reeling trying to figure out: What are those downstream impacts?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF, the independent source for health policy research, polling and journalism.