AROUND 7,500 women are diagnosed with ovarian cancer each year in the UK and 4,100 pass away from it.
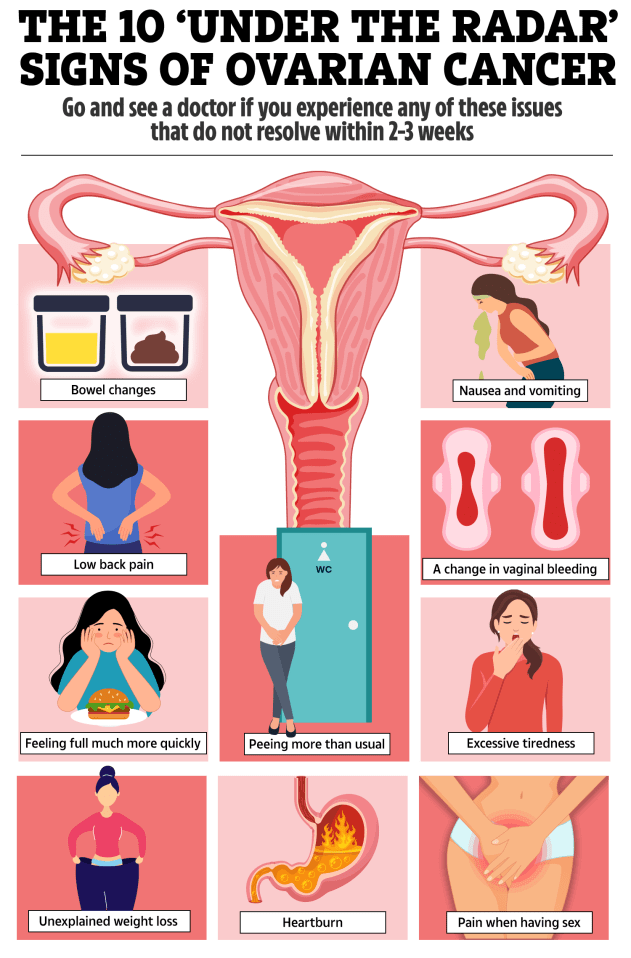
But symptoms of the disease – which is the sixth most common cause of cancer death in women – can be difficult to spot, often remaining subtle until the cancer has developed.
On top of that, the signs of ovarian cancer can be easily confused with other conditions, Dr Alexis Missick, a GP working with pharmaceutical company UK Meds, warned.
The cancer can cause sufferers pain in the pelvic area, but it can also affect their toilet habits.
One telltale sign might even make itself known at the dinner table.
Ovarian cancer affects the ovaries, two small glands that form of part of the female reproductive system.
Read more on ovarian cancer
The ovaries produce, store, and release eggs for reproduction and are also responsible for making the female sex hormones oestrogen and progesterone.
Ovarian cancer starts when abnormal cells in and around the ovary and fallopian tubes grow and divide in an uncontrolled way and form a cancerous tumour.
The cancerous cells grow into surrounding tissues and can spread to other parts of the body.
The most common type of the disease is epithelial ovarian cancer, which starts in cells covering the surface of the ovary.
There are other less common types, such as germ cell tumours and stromal tumours.
Ovarian cancer is most common in women over 50, particularly those who have gone through menopause. However, it can also affect younger women.
Risk factors include having a family history of ovarian or breast cancer, certain genetic mutations, and never having been pregnant.
Women who have used hormone replacement therapy (HRT) after menopause may also have a higher risk, according to Ovarian Cancer Action.
As March marks ovarian cancer awareness month, Dr Missick revealed four silent symptoms of the cancer:
- Bloating or swelling of the abdomen
- Pelvic pain or discomfort
- Feeling full quickly when eating
- Needing to pee more often and more frequently
“There are other, more unusual symptoms of ovarian cancer which people may not commonly associate with cancer,” the GP went on.
These include:
“Since these symptoms can overlap with less serious conditions they can be easy to ignore,” Dr Missick noted.
“If you experience any of these persistently and in tandem with more common symptoms, then it is worth seeking advice from your doctor or GP,” she stressed.
Who’s at higher risk of ovarian cancer?
There are a few factors that can increase the risk of developing ovarian cancer.
- Age: The risk of ovarian cancer increases with age and is most commonly diagnosed in older adults.
- Genetics: If you have blood relatives who have previously been diagnosed with ovarian cancer then there is an increased risk of the disease.
- Gene changes: Some cases of ovarian cancer are caused by gene changes inherited from your parent. The BRACA1 and BRACA2 genes can increase the risk of ovarian cancer and breast cancer.
- Endometriosis: If you suffer from endometriosis you may be more at risk of ovarian cancer as tissue similar to the tissue inside the uterus, grows on the outside of the uterus.
- Being overweight: Obesity can increase the risk of ovarian cancer.
How is ovarian cancer treated?
Dr Missick said: “The treatment for ovarian cancer is completely dependent on the stage and type of ovarian cancer you are diagnosed with and you will be advised on the best option by your doctor.
“Some treatment options include surgery to remove as much of the cancer as possible, chemotherapy to shrink the tumours and hormone therapy.
“It is important to have thorough discussions with your doctor about the best course of treatment.”
Ovarian cancer can be serious, especially if it’s diagnosed at a late stage. However, when diagnosed at stage 1, 90 per cent of women live beyond five years.
The outcome depends on several factors, including the stage of the cancer when it’s found, the type of ovarian cancer, and how well it responds to treatment.
Last year, University of Oxford scientists said they were creating a vaccine that teaches the immune system to recognise and attack the earliest stages of ovarian cancer, “wiping out” the disease.
The hope is that the shot could be given to women preventatively on the NHS with the aim of eliminating the disease.
Experts suggest it could work in a similar way to the human papillomavirus (HPV) jab, which is on track to stamp out cervical cancer.
HPV jabs are currently dished out to secondary school children and people at high risk of the virus, cutting their risk of getting conditions linked to HPV – including cervical cancer and genital warts.