THE husband of a vegan mum who was “obsessed with hygiene” and died from a horror E coli infection has paid tribute to her.
Laura Farmer, 46, died at a London hospital in April after being diagnosed with Hemolytic-uremic syndrome (HUS), caused by Shiga toxin-producing E coli (STEC).
Her husband of 14 years, Steve Farmer, wrote about the “powerhouse of a woman” and told the story of how they met, in a touching tribute following her tragic death.
In a post on April 30, he revealed how he sold her a bike, and then went on a run for their first date, before he proposed to her – with a ring that didn’t fit – a few months later.
He wrote: “We travelled the world, we bought a house, she taught me to scuba dive, we learned to ski.
“She gave birth to [our son], a daredevil of fun and kindness, and we began our next episode.
“I opened many a bottle of fizz for her, she called it attitude changer, sundowner, or just because!
“We made up parenting as we went. That’s a lie, she researched it, wrote lists and smashed it out the park.”
But he revealed how, the previous Friday, he lost “the most amazing woman way too soon”.
He added: “In honour of Laura, go watch the ducklings, write your affirmations, make healthy choices, break them!
“Have a sundowner and love every second of your journey.
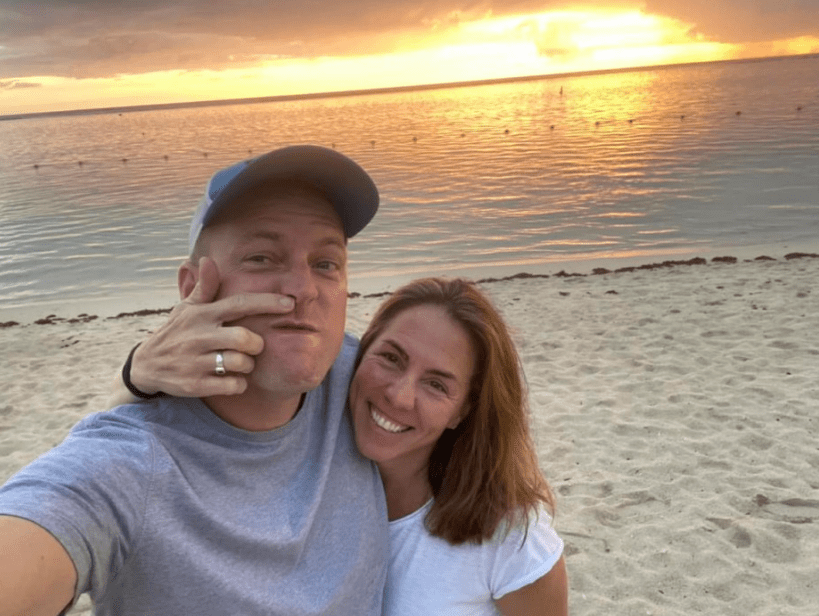
“She would laugh, smile and nod at my picture choice… warm sea full of fish, sun on her back, sundowner consumed and taking the P out of me.”
Coroner for Inner North London, Mary Hassell, said Laura was conscious about food hygiene, and the family found the E coli diagnosis “difficult to understand”.
The coroner added: “She was a vegan who took great pains with food preparation.
“As a family they were extremely hygiene conscious.
“When Ms Farmer became ill, her family members wanted to understand what had happened and to keep themselves as safe as possible.”
A jury made a determination at inquest that Laura Farmer died from a stroke caused by an E coli infection.
What are the symptoms of STEC?
Shiga toxin-producing Escherichia coli can cause gastrointestinal illness that can become severe.
The most common type of STEC in the UK is O157, according to a 2017 report by Public Health England.
Some people who are exposed to STEC do not become ill. Others develop stomach cramps and bloody diarrhoea.
Symptoms can also include vomiting, fever, and chills.
In severe cases, the infection can damage organs, such as the kidneys.
Symptoms can appear anywhere from one to ten days after exposure but usually appear around three to four days after exposure.
Most of those affected by the bug will get better without treatment within a week. Sufferers are advised to drink plenty of fluids to stay hydrated.
Are you at risk of getting it?
People can become infected by:
- Eating contaminated food
- Contact with infected animals either directly or through inadvertent contact with animal faeces, for example at farms, petting farms and campsites
- Contact with other people who have the illness (through inadequate hand hygiene after using the toilet, before food handling – particularly in households, nurseries, infant schools, or both
- Drinking water from inadequately treated water supplies
- Swimming or playing in contaminated water such as ponds or streams
STEC are very infectious because very few bacteria are needed to cause illness.
This means that disease can spread easily within families and in other settings such as day nurseries, primary schools, nursing homes and hospitals where there are young children and others who might have difficulty keeping clean.
How can you protect yourself from STEC?
An STEC infection can be prevented by taking the following precautions:
- Cook all minced meat products (burgers, meatloaf, meatballs) thoroughly, until the colour is the same all the way through, and no blood runs from them
- Ensure refrigerators are working correctly – bacteria grow more quickly at temperatures over 4oC
- Only leave cooked foods, meat and dairy products out at room temperature for a short time
- Store uncooked meats below-cooked meats and salad vegetables to avoid dripping juices onto ready-to-eat food
- Store uncooked and cooked meats on different plates, and avoid all contact between raw and cooked meats
- Thoroughly wash all salad vegetables and do not prepare them with utensils that have also been used for raw meat
- Children and the elderly who are particularly susceptible to the severe effects of STEC should avoid eating or drinking unpasteurised dairy products
- People who have been ill should not prepare food for others for at least 48 hours after they have recovered
- Boil any drinking water if you are unsure of its source
- Do not swim in water that you think may be contaminated by cattle and sheep in nearby fields
- Wash your hands thoroughly after using the toilet (or helping others including changing nappies), handling raw meat, before meals and after contact with animals
Source: PHE
Ms Farmer was admitted to University College Hospital on 20 April and diagnosed with HUS caused by Shiga toxin producing E coli.
When she was “thought to be in the recovery phase”, she suffered an unexpected stroke and, despite best efforts, died as a consequence, according to the Prevention of Future Deaths Report.
The coroner listed matters of concern, saying there was a risk that future deaths would occur “unless action is taken”.
She wrote: “After his wife’s diagnosis, Mr Farmer was given no advice about how to keep himself and their child safe.
“He cleaned the bathroom in anticipation of his wife’s return home, but did not use any personal protective equipment.
“When he later became unwell, he did not know whether he had put himself at risk.
“Having heard his description in court, I think it is not an exaggeration to say that he was then terrified that his own actions might leave his child an orphan.
“The clinicians treating Ms Farmer gave evidence at inquest that they did not know if the source of the infection that killed her had ever been identified.”
In her matters of concern, the coroner wrote that someone from “what was described to me as public health (I assume the UKHSA)” spoke to Laura the day before her death.
They asked for information, but she was in intensive care and not able to give a full, detailed picture.
“There was apparently no exploration of potential contact with animals or water sports and I was told that only scant details of a recent restaurant visit were obtained,” she wrote.