There are around 8,000 deaths from oesophageal cancers in the UK each year, accounting for five per cent of all cancer deaths.
But now a team of experts from universities and hospitals have developed a technique to detect and diagnose in seconds.
The project, led by Professor Nick Stone at the University of Exeter, is called RaPIDE.
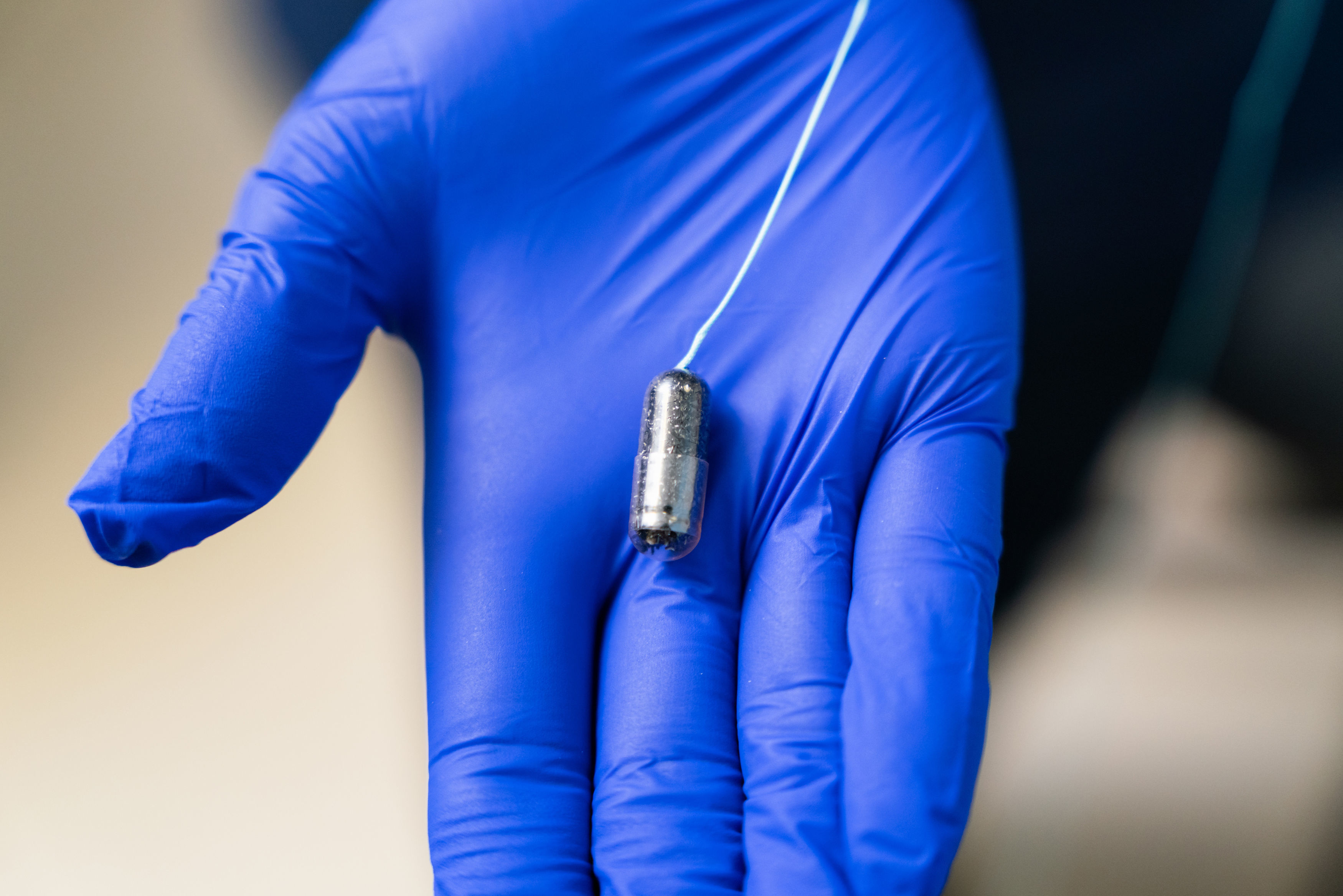
New medical devices developed use light to pinpoint cancerous tissues or cells almost instantaneously, using a laser-based technique called Raman spectroscopy.
Current diagnoses can take two weeks, but they new approach could cut that to under 30 seconds.
They hope the test will leader to quicker and more accurate tests which will improve health outcomes.
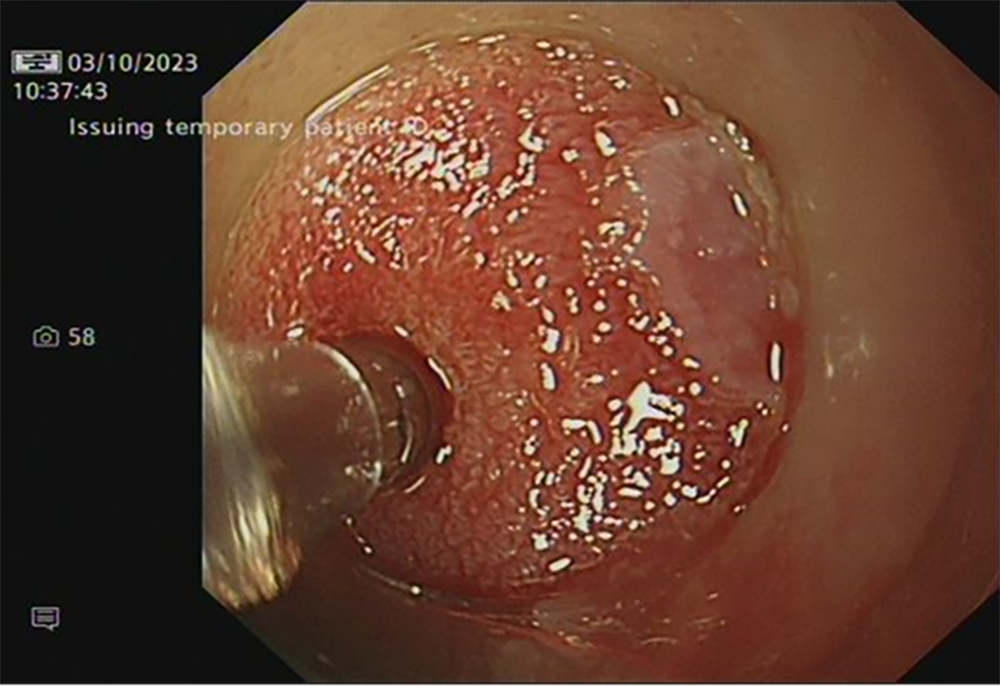
RaPIDE allows medical experts to measure the light scattered by tissues when a low-power laser is shone onto it.
The light changes if it is on healthy or diseased tissues, meaning pre-cancerous or cancerous tissues can be detected rapidly.
They are able to do the test both inside the patient’s throat and also on biopsied tissues.
Signals from the probe are analysed by a computer and can be processed by the latest AI to aid the clinician’s decisions.
The research team have started undertaking clinical trials involving patients, with 19 tested so far.
Oliver Old, Consultant Upper GI Surgeon from Gloucestershire Hospitals, said: “We are excited by the prospect of introducing this new technology to benefit patients.
“This technology can help us to target these early cancers more accurately, improving cure rates and reducing the need for major surgery.”
Oesophageal cancers are the seventh most deadly in the UK as they are often discovered late due to minimal symptoms, making successful treatment difficult.
Dr Alex Dudgeon, Research Fellow at the University of Exeter said “If we can diagnose cancers and other abnormal changes with our device in seconds, without removing any tissue, this would revolutionise the field, saving time and the NHS money.
“With an instant diagnosis, treatment can be started earlier which will improve patient outcomes.”
The group are also seeing whether the technique can identify lymphomas and neuromuscular diseases.
RaPIDE stands for: Raman Probe for In-vivo Diagnostics (during oesophageal) Endoscopy.
The group is from University of Exeter, University of Bristol, and Gloucestershire Hospitals NHS Foundation Trust.
The study was funded by the National Institute for Health and Care Research – the research partner of the NHS.
The AI technology that could already save your life
THE NHS AI Lab has also been set up to co-ordinate Government, health providers, academics and tech firm any promising innovations.
Tara Donnelly, the former chief digital officer of NHS England, is now the founder of health advisory firm Digital Care, which helps the NHS scale tech.
She said: “Most weeks there is exciting news of a potential breakthrough in AI in health.
“For example, at Moorfields Eye Hospital in London, the AI system can recommend the correct referral decision for over 50 eye diseases with 94 per cent accuracy, matching world-leading eye experts.”
One reason the NHS is so suited to the use of AI is that it treats almost 1.3million people a day.
That can mean long waiting lists and A&E waits but is also an advantage when it comes to AI, because those patients produce a lot of data.
And it’s data that AI learns from, to make sure it works optimally.