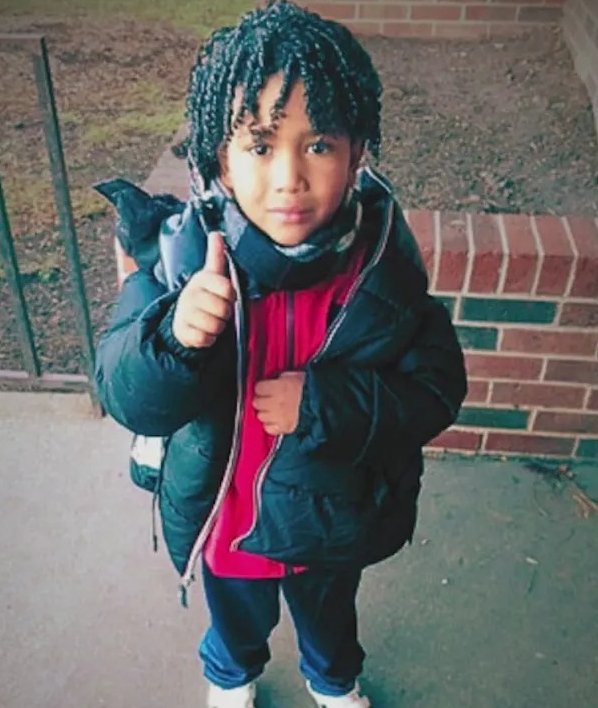
Jean Carlos Martinez Rivero was staying at migrant shelter in Chicago when he was rushed to hospital in December last year.
The Chicago Department of Public Health initially stated that Jean had died from a medical emergency.
But a report release almost two months after his death confirmed sepsis as the cause, which Jean developed after contracting a Group Strep A infection and Covid-19.
Two other viruses played a role in his death, the report further revealed.
Dr Juanita Mora, an allergist and immunologist, told NBC Chicago: “It’s too much for a little body. It really is sad.
“We have to remember that a 5-year-old has a very small amount of volume when it comes to bodily fluids.
“So, when an overwhelming infection like COVID-19 hits his body, and at the same time he gets strep throat, it starts going into the blood stream, it starts affecting the rest of the organs.”
Responding the medical examiner’s report on Jean’s death, Chicago mayor Brandon Jonhsnon office released a statement expressing it’s “deepest condolences” to the little boy’s family.
“This is a tragic loss,” it added.
“The report issued by the Cook County Medical Examiner determined that the cause of death was sepsis, a rare complication due to invasive Streptococcus pyogenes, also known as Group A Strep, that rapidly became fatal,” the mayor’s press office explained.
“Sepsis can lead to serious complications in as little as 24 hours.
“Ambulance services were called immediately when the family reported a medical emergency.
“Shelter staff performed chest compressions on the child but he tragically died shortly after arriving at the hospital.”
Streptococcus pyogenes are bacteria commonly found in the respiratory tract and skin that can cause milder illnesses like sore throat, fever and skin infections.
It can also cause tonsillitis, cellulitis, impetigo – a very contagious infection that starts with blistered skin – and scarlet fever, which is flu-like and tends to occur in children.
It can be serious if not treated swiftly with antibiotics.
However, in rare cases, the bacteria can trigger invasive Group Strep A infection if they enter the lungs or bloodstream.
These infections can be life-threatening and even fatal.
The UK saw an increase in invasive Group Strep A infections in December last year, resulting in the deaths of children.
More kids sickened
Officials from the city’s fire department told NBC Chicago that they took other sick children from the same shelter Jean was in to the hospital in the week after the five-year-old passed away.
Dr Mora said viruses and bacteria spread easily in shared living spaces like shelters.
She added that she’d seen many children with a strep infection this season and that it’s likely Jean experienced symptoms from it leading up to his death.
“I always tell parents to watch for three things: One, fever that doesn’t resolve. Two, fatigue, a child that is sleeping a lot and three, loss of appetite,” Dr Mora said.
What are the symptoms of a Strep A infection?
According to the NHS, common symptoms of strep A include:
- flu-like symptoms, such as a high temperature, swollen glands or an aching body
- sore throat (strep throat or tonsillitis)
- a rash that feels rough, like sandpaper (scarlet fever)
- scabs and sores (impetigo)
- pain and swelling (cellulitis)
- severe muscle aches
- nausea and vomiting
Most Strep A infections aren’t serious and can be treated with antibiotics.
But rarely, they may develop an invasive group A strep infection.
When it comes to your child, you should contact NHS 111 or your GP if:
- Your child is feeding or eating much less than normal
- Your child has had a dry nappy for 12 hours or more or shows other signs of dehydration
- Your baby is under 3 months and has a temperature of 38C, or is older than 3 months and has a temperature of 39C or higher
- Your baby feels hotter than usual when you touch their back or chest, or feels sweaty
- Your child is very tired or irritable