Lucy Walton was aged 26, single, and in the depths of what she called “the panic years” when she joined a growing number of Australians testing their fertility.
Key points:
- Fertility testing is becoming more accessible as demand grows
- Experts say some patients are concerned about how their age impacts fertility as the average age of first-time mothers in Australia increases
- Patients are cautioned against unethical fertility tests that are pushed by commercial interests
“It was the classic: ‘Should I be travelling? Should I be settling down? Should I just be having fun?” she said.
“I just wanted to get everything checked to know whether having kids would be something that was easy for me or challenging,” she said.
Until recently, fertility testing was considered an onerous, expensive, and time-consuming process that was mostly reserved for the one in six couples experiencing infertility or pursuing in-vitro fertilisation (IVF).
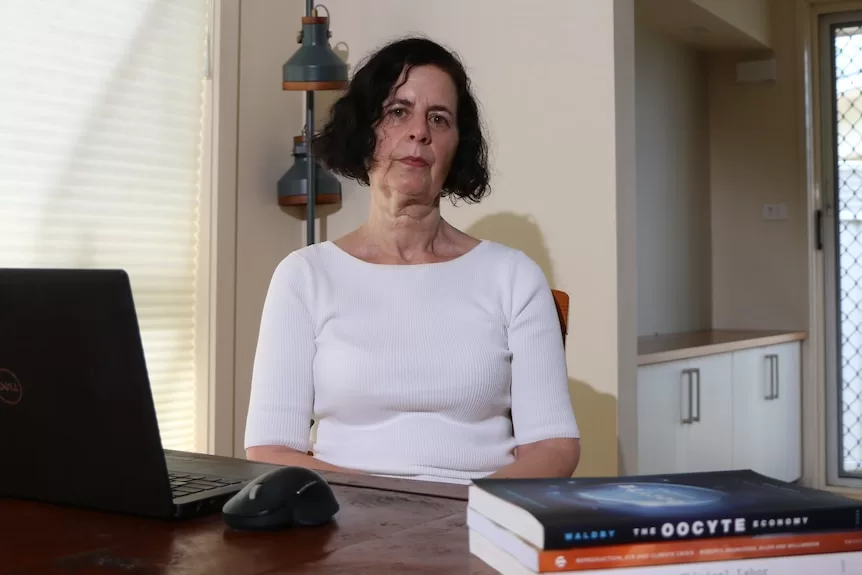
“However, what has happened recently is that one of the standard tests, which is the Anti-Mullerian Hormone (AMH) test, has become more generally available,” ANU sociologist Professor Catherine Waldby said.
It involves a blood test that can measure AMH levels to determine the number of eggs in a patient’s ovaries.
Happily in Ms Walton’s case, the blood test gave her the result she was after — there were no obvious signs of fertility issues.
Average age of first-time mothers likely to keep rising
ABC News: Luke Stephenson
)
AMH tests can be done through a general practitioner or at an IVF clinic, but a surge in demand has produced a market of relatively cheap at-home fertility kits.
“So we can tell simply by the fact of availability, and the fact that there is now more and more of a market for this test, that it is being taken on,” Professor Waldby said.
According to Australian government data produced by the Centre for Population, the top four factors influencing fertility decisions are: the costs of raising children, careers, relationships, and the cost of housing.
Professor Waldby said COVID-19 and the rising cost of living had seen it take longer and become “more and more expensive” for people to establish the right pre-children conditions.
That means the average age of first-time mothers in Australia is likely to continue to rise, after increasing from 28.7 in 2011 to 29.7 in 2021, according to the Australian Bureau of Statistics.
“What that means is your fertile window is getting narrower,” she said.
Test determines quantity not quality
ABC News: Marco Catalano
)
Since Professor Kelton Tremellen introduced the AMH test in Australia two decades ago, he has witnessed a surge in demand from women, like Ms Walton, who are worried about how their age can impact fertility.
“There are now more actions a woman can take if she were to have low results,” he said.
“A lot of women are freezing their eggs before they’re in a social position to have a family … others would bring forward their plans to have kids.”
But Professor Tremellen said the test was not to be mistaken as a way of adding time to a biological clock.
“It is not a good marker of egg quality, it is merely a marker of egg number,” he said.
“It just personalises your situation and can help make decisions.”
Concerns unethical players are using panic to sell fertility procedures
Egg-freezing was initially invented to help cancer patients preserve their eggs.
However, egg-freezing for non-medical purposes has increased in uptake by 56 per cent between 2020 and 2021, according to data from the Australia and New Zealand Assisted Reproduction Database.
“The idea is that you freeze them when you’re in your late 20s or early 30s and then you are more able to wait for the right partner, the right house, the right job … whatever it is you need to create the conditions to have a child,” Professor Waldby said.
“But there are now a lot of commercial interests moving into this field, and this is reshaping the area very profoundly.”
The price of egg-freezing for non-medical purposes is not covered by Medicare, and can cost patients around $10,000 per cycle, with some clinics encouraging up to three cycles.
“There’s the risk that you may never go back and use these eggs … and you have the baby that you want in a normal way,” Professor Waldby said.
She said she was also concerned that commercial entities were pushing the idea of routine fertility testing and egg collection by driving a sense of rising panic.
“We can locate a lot of this stuff in the bigger trend towards wellness and self-monitoring,” she added.
“Certainly in the United States, you get quite aggressive marketing to women [with the] suggestion that if they don’t do all these things, they’ll potentially find themselves unable to have kids.”
Professor Tremellen has warned against services that offer fertility tests without expert interpretation.
“That is poor practice … you can imagine a low result can create a huge amount of anxiety for a patient,” he said.
But with the right medical expertise, Professor Tremellen said fertility testing can offer a personalised reproductive status beyond mere age.
“Some of these companies are quite reasonable, they’re backed by very eminent fertility gynaecologists,” he said.
“And once the patient has a result, they will have some counselling, which I think is mandated.
“So [fertility test results] need to be interpreted in real time, in front of a doctor, where they can put it all together and give the patient some idea of what it really means and what options they have going forward.”